
Managing Metabolic Syndrome with Telehealth

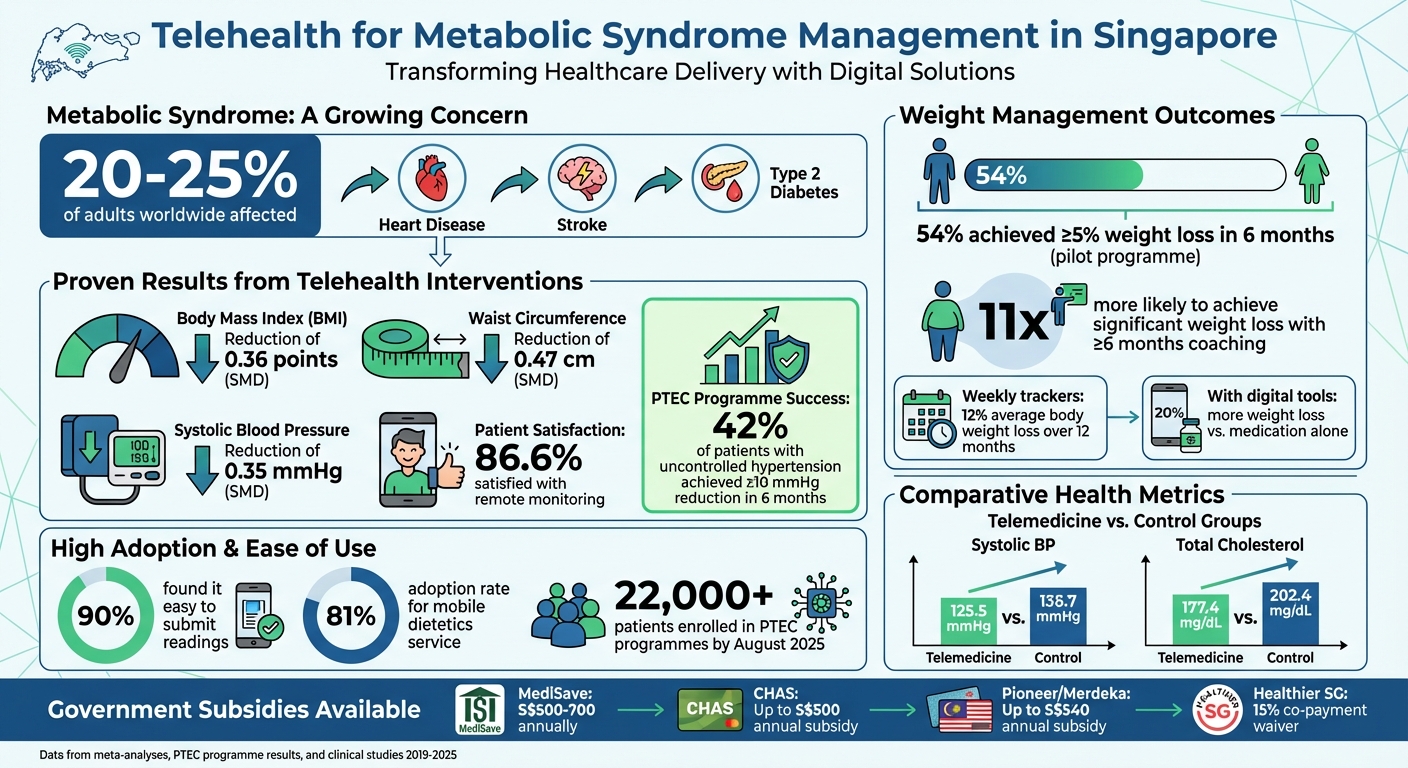
Metabolic syndrome is a growing health concern, affecting 20–25% of adults worldwide and increasing risks of heart disease, stroke, and type 2 diabetes. In Singapore, telehealth is reshaping how this condition is managed, making care more accessible and convenient.
Here’s how telehealth is improving metabolic syndrome management:
- Remote Monitoring: Tools like Bluetooth-enabled devices send real-time data (e.g., blood pressure, glucose) to healthcare teams, reducing clinic visits.
- Integrated Care: Patients can consult doctors, dieticians, and physiotherapists via digital platforms, streamlining access to multiple specialists.
- Personalised Treatment: Programmes like Trimly provide tailored weight management plans, including GLP-1 medications delivered to your doorstep.
- Improved Outcomes: Studies show telehealth reduces BMI, waist circumference, and blood pressure while boosting treatment adherence.
With government support through subsidies like MediSave and CHAS, telehealth is a practical option for managing metabolic syndrome efficiently and affordably.
Telehealth Impact on Metabolic Syndrome: Key Statistics and Outcomes in Singapore
The Data Is In: Reversing Metabolic Disease Is Possible
How Telehealth Changes Metabolic Syndrome Management
Telehealth is revolutionising the way Singaporeans manage metabolic syndrome by bringing care directly into their homes. Instead of juggling multiple clinic visits to see various specialists, patients can now connect with their entire care team - doctors, nurses, dieticians, and physiotherapists - through digital platforms. This eliminates the hassle of travelling to clinics and ensures continuous monitoring and timely interventions. It’s a game-changer for chronic disease management.
More than just convenience, telehealth enhances patient adherence. With tools for real-time monitoring of vital signs, medication adjustments, and quick responses to any issues, it bridges the gaps left by traditional episodic care, where problems might go undetected for longer periods.
Main Benefits of Telehealth for Chronic Conditions
The Primary Tech-Enhanced Care (PTEC) programme is a great example of how telehealth is transforming chronic disease management. Launched in July 2019 at Ang Mo Kio Polyclinic, this pilot programme involved 120 patients and delivered impressive results. Participants used Bluetooth-enabled blood pressure monitors that automatically sent readings to their care team. Over six months, 42% of patients with previously uncontrolled hypertension saw their systolic blood pressure drop by at least 10 mmHg. On top of that, 90% of participants found it easy to submit their readings, showcasing how user-friendly the system is.
The programme also featured a bilingual SMS chatbot that provided interactive advice on self-care, tips for a healthy lifestyle, and guidance for handling high readings. This combination of automated monitoring and real-time support kept patients actively engaged with their treatment plans.
"Healthcare providers also feel more confident about replacing a physical visit by the patient with a tele-consultation because of remote monitoring and continual engagement." – Associate Professor Chong Phui-Nah, CEO, National Healthcare Group Polyclinics
Platforms like Trimly further highlight the potential of telehealth. They offer remote, doctor-led consultations focused on tailored weight management, an essential component of metabolic syndrome care. Through video consultations, patients receive personalised treatment plans, including GLP-1 medications, with prescriptions delivered straight to their homes. This model is especially beneficial for busy professionals or those with mobility challenges, ensuring they can stick to their treatment plans without disruptions.
Using Technology for Monitoring and Support
Modern telehealth systems go beyond consultations by incorporating devices like glucose metres and weight scales, which automatically send data to healthcare teams. This real-time information allows providers to make immediate adjustments to treatments, preventing small issues from becoming bigger problems.
Digital tools also play a key role in keeping patients engaged. SMS chatbots, for example, offer advice based on clinical guidelines, send reminders for measurements, and encourage healthy lifestyle habits. For patients managing multiple risk factors - such as high blood pressure, elevated glucose levels, and excess weight - these tools provide continuous support, reducing the need for frequent clinic visits.
Research backs up the effectiveness of these digital solutions. A meta-analysis of eHealth interventions for metabolic syndrome reported measurable improvements, including reductions in Body Mass Index (SMD = −0.36), waist circumference (SMD = −0.47), and systolic blood pressure (SMD = −0.35). These findings show that digital platforms not only make healthcare more accessible but also improve outcomes by helping patients stick to their treatment plans more effectively.
Complete Care Delivery Through Telehealth
Telehealth takes the convenience of real-time monitoring a step further by bringing together multiple specialists into a single, cohesive care process. Managing metabolic syndrome often requires input from a variety of healthcare professionals, and telehealth bridges this gap by connecting patients with their care team remotely. Instead of juggling separate appointments with a dietician, psychologist, and physiotherapist, you can now access all these services from the comfort of your home. This approach directly addresses the scheduling and logistical challenges of traditional care.
For busy professionals and caregivers, this streamlined solution is a game-changer, making comprehensive care more manageable.
Access to Multiple Healthcare Professionals
Telehealth platforms provide access to a diverse range of specialists, including family physicians, dieticians, psychologists, physiotherapists, and nurses trained in managing chronic conditions like metabolic syndrome. Each professional focuses on a specific aspect of your health, ensuring a well-rounded approach to treatment.
- Tele-Dietetics: Dieticians can create meal plans tailored to your home environment and kitchen setup. For instance, at National University Hospital, a mobile dietetics service saw an impressive 81% adoption rate.
- Tele-Psychology: Mental health support is crucial for patients navigating lifestyle changes or dealing with emotional eating. Telehealth makes this support easily accessible.
- Tele-Physiotherapy: Through video consultations, physiotherapists guide patients in staying active without requiring gym memberships or in-person sessions.
This integrated network allows for more personalised and effective care strategies.
Coordinated and Personalised Treatment Plans
The true strength of telehealth lies not just in access but in how seamlessly these specialists work together. Digital platforms enable your care team to share patient data effortlessly, ensuring coordinated follow-ups and a unified treatment approach.
A study on telemedicine for metabolic syndrome highlighted its effectiveness: patients achieved lower systolic blood pressure (125.5 mmHg compared to 136.7 mmHg in control groups) and reduced total cholesterol levels (177.4 mg/dL versus 202.4 mg/dL). Additionally, 86.6% of patients reported satisfaction with remote monitoring.
Nurses specialising in chronic disease management play a key role by handling medication adjustments and follow-ups through video consultations. This allows doctors to focus on more complex cases while ensuring timely care for all patients. Continuous Bluetooth monitoring enables the care team to detect and address potential issues before they worsen.
The impact of telehealth is evident in weight management outcomes. Patients who engaged in at least six months of app-based coaching were 11 times more likely to achieve clinically significant weight loss (≥5%) compared to those with shorter coaching durations. In one pilot programme, 54% of participants achieved ≥5% weight loss within six months, showcasing the measurable benefits of coordinated, personalised care through digital platforms.
Medication Management and Remote Monitoring in Telehealth
Telehealth simplifies medication management for metabolic syndrome by reducing the need for frequent clinic visits. This approach makes accessing and managing medications much easier.
Direct Medication Delivery
In Singapore, telehealth providers offer comprehensive services that remove the need for physical trips to pharmacies. After a video consultation with a licensed doctor, eligible patients can have their prescriptions delivered straight to their homes. This discreet and convenient process is especially helpful for those seeking weight management treatments.
Currently, Singapore has approved eight GLP-1 medications for managing weight and diabetes. These include Saxenda and Wegovy for weight loss, and Ozempic and Rybelsus for diabetes treatment. For instance, Saxenda is approved for individuals with a Body Mass Index (BMI) above 30, or for those with a BMI over 27.5 if they have chronic conditions like high blood pressure or high cholesterol. To ensure safety, telehealth providers verify patient details during video consultations and may even request patients to film themselves on a weighing scale to confirm their BMI.
"We have a very strong commitment towards ensuring that the patient is deemed to be suitable for the medication by a qualified doctor." - Rio Hoe, Co-founder, Ease Healthcare
Telehealth providers report that 20% to 40% of GLP-1 requests are rejected, often because patients do not meet the required BMI criteria. This careful screening ensures medications are prescribed only to those who truly need them. Platforms like Trimly combine GLP-1 prescriptions with remote monitoring for conditions like hypertension and high cholesterol, offering personalised treatment plans starting at S$350+ per month. These plans include free unlimited follow-ups and medication delivery, enhancing the integrated care offered through telehealth.
Remote Monitoring for Better Treatment Adherence
Telehealth doesn’t just stop at medication delivery - it also supports ongoing care through remote monitoring, which is key to maintaining treatment adherence. Bluetooth-enabled devices automatically send vital health readings to care teams, enabling timely adjustments to medications without requiring in-person visits. This real-time data sharing ensures that treatment plans adapt to a patient’s needs as they arise, rather than waiting for scheduled appointments.
Tracking progress regularly has clear benefits. A study published in Obesity Science and Practice in January 2025 examined 66,094 members of the Found Health telehealth platform. It found that members who logged their weight weekly for 12 months lost an average of 12% of their body weight. Those who used digital behaviour change tools achieved 20% more weight loss compared to those relying on medication alone. Patients who actively track their progress and engage with their care teams often experience much better outcomes overall.
sbb-itb-5db499f
Telehealth in Singapore's Healthcare System
Telehealth is transforming how metabolic syndrome is managed in Singapore, thanks to its focus on remote monitoring and personalised care. The government plays a key role in this transformation by incorporating telehealth into national healthcare programmes. For instance, the Chronic Disease Management Programme (CDMP) covers 23 chronic conditions, including diabetes, hypertension, and hyperlipidaemia, ensuring that telehealth consultations receive the same subsidies and support as traditional clinic visits.
Integration with Government Healthcare Programmes
The Ministry of Health's Office for Healthcare Transformation (MOHT) has introduced initiatives like the Primary Tech-Enhanced Care (PTEC) programme, which allows patients to monitor their health from home using Bluetooth-enabled devices. By August 2025, the PTEC Home Blood Pressure Monitoring Programme had expanded to all polyclinics. Led by Clinical Director Professor Gerald Koh, the programme enables patients to send health data directly to polyclinic care teams, who then provide clinical advice through tele-consultations. This initiative, along with the Home Diabetes Monitoring Programme, has already enrolled over 22,000 patients.
The Healthier SG initiative, launched in 2023, takes telehealth integration a step further. It ensures seamless care coordination between primary care providers and specialists via integrated Clinic Management Systems (CMS). Patients can also benefit from services like "Tele-Dietetics" and "Tele-Physiotherapy", which provide lifestyle guidance remotely. Additionally, MOH-approved telehealth providers offer personalised care plans, including GLP-1 medications and unlimited follow-ups, all through online platforms. These efforts not only improve access to care but also align telehealth with broader healthcare strategies.
Lower Costs with CHAS Subsidies
Affordability is another key factor driving the adoption of telehealth for chronic conditions like metabolic syndrome. Government subsidies make telehealth consultations more accessible. For example, under the MediSave 500/700 Scheme, patients can use up to S$500 annually for non-complex chronic conditions or S$700 for complex ones (involving multiple conditions or complications). CHAS cardholders enjoy up to S$500 in annual chronic care subsidies, while Pioneer Generation and Merdeka Generation cardholders receive enhanced subsidies of up to S$540 per year.
Since 1 February 2024, patients enrolled in Healthier SG have benefited from a waiver of the standard 15% cash co-payment for CDMP treatments. This makes telehealth consultations even more affordable, allowing patients to fully utilise their MediSave funds without additional costs. Furthermore, MediSave can be used for allied health services, such as dietician consultations, which are crucial for managing metabolic syndrome through lifestyle changes.
| Programme/Subsidy | Coverage/Benefit | Eligibility |
|---|---|---|
| CDMP | Covers 23 conditions (e.g., diabetes) | All eligible Singaporeans |
| MediSave 500/700 | S$500–S$700 annual outpatient limit | MediSave account holders |
| CHAS Chronic | Up to S$500 annual subsidy | CHAS Blue/Orange/Green cardholders |
| Pioneer/Merdeka Gen | Up to S$540 annual subsidy | PG/MG cardholders |
| Healthier SG | 15% co-payment waiver for CDMP treatments | Enrolled Healthier SG patients |
Weight Loss and Long-Term Health Outcomes with Telehealth
Practical Weight Loss Goals for Metabolic Syndrome
Even a modest reduction in weight can lead to better blood pressure, blood sugar, and cholesterol levels. You don’t need a dramatic transformation - research indicates that losing just 5% to 10% of your body weight can significantly improve these metrics. In fact, even a 2% weight loss can make a noticeable difference in reducing health risks.
Tools like digital scales, logging apps, and video consultations can play a big role in helping you achieve these goals. Studies show that eHealth interventions can lower Body Mass Index by an average of 0.36 points, reduce waist circumference by 0.47 cm, and decrease systolic blood pressure by 0.35 mmHg.
MOH-approved telehealth clinics like Trimly offer personalised plans that combine doctor-led guidance with GLP-1 medications to target both short-term weight loss and long-term metabolic health. These medications have shown impressive results, with Semaglutide reducing weight by up to 15.8%, Tirzepatide by up to 22.5%, and Liraglutide by up to 6%. Delivered straight to your home and monitored remotely, these treatments provide a convenient option for managing metabolic syndrome in Singapore.
However, reaching your weight loss goal is just the beginning - consistent effort is needed to maintain these benefits over time.
Continued Support for Preventing Complications
Once weight loss goals are achieved, ongoing telehealth support is key to preventing complications. For instance, between December 2019 and July 2020, Northwestern Medicine ran a telehealth programme in Chicago for 80 patients with a BMI ≥27 and at least one cardiovascular risk factor. Using cellular-enabled smart scales and personalised messaging, the programme, led by Dr Ronald T. Ackermann, showed that 60% of participants lost weight within six months, and 15% managed to lose 5% or more of their body weight.
"Achieving and maintaining weight loss is difficult... Adults are more likely to achieve weight loss and activity goals when supported by behavioural interventions involving recurring contact with a behavioural coach." – Ronald T. Ackermann, MD, MPH, Northwestern University
Another major study published in January 2025 in Obesity Science and Practice tracked 66,094 members of a virtual weight-loss platform. The findings were compelling: members who engaged weekly for 12 months lost an average of 10% of their body weight, and 83% of those who saw early progress maintained their weight loss for at least a year. Weekly weight tracking led to an average loss of 12%, while those who actively worked with clinicians and coaches experienced 20% more weight loss compared to those relying solely on medications.
Sustaining weight loss and managing metabolic syndrome require ongoing support and accountability. Telehealth platforms make this easier by enabling regular follow-ups and collaboration among specialists, including endocrinologists, dietitians, and psychologists. These tools also allow for real-time monitoring of vital signs like blood pressure and heart rate, helping providers identify potential issues early and adjust treatment plans as needed. This level of continuous care is hard to match with traditional quarterly clinic visits.
Conclusion
Managing metabolic syndrome has become far more convenient with telehealth, reducing the need for frequent clinic visits. By combining remote monitoring with digital tools, telehealth provides medical supervision and personalised care that fits seamlessly into your daily routine. These platforms offer consistent, tailored care without the hassle of constant in-person appointments.
Research highlights the effectiveness of telehealth in improving key health metrics like BMI, waist circumference, and blood pressure, all while maintaining high patient satisfaction. In Singapore, programmes such as the Primary Tech-Enhanced Care pilot at Ang Mo Kio Polyclinic have shown promising outcomes - 42% of patients with poorly controlled hypertension experienced a drop of at least 10mmHg in systolic blood pressure within six months. These results underscore the practical benefits of remote care.
For those seeking a structured, doctor-led approach to managing weight and metabolic health, MOH-approved platforms like Trimly offer personalised treatment plans under medical supervision. This approach combines convenience with professional oversight, making it easier to stay on top of your health goals without disrupting your daily schedule.
Telehealth is transforming how we manage metabolic health, giving you the right support exactly when you need it.
FAQs
How can telehealth help patients manage metabolic syndrome more effectively?
Telehealth has transformed how metabolic syndrome is managed, making it both easier and more accessible by seamlessly fitting care into daily routines. With digital tools, doctors can send reminders for medications, keep an eye on blood pressure or glucose levels, and assess lifestyle data in real-time. This kind of instant feedback helps patients stay on track, all without the hassle of frequent clinic visits.
For those using Trimly, the clinic’s fully online, doctor-led service takes convenience a step further. Patients benefit from personalised treatment plans, unlimited virtual consultations, and medications delivered straight to their doorstep. The app also keeps things on track with features like GLP-1 injection reminders and meal tracking. By cutting down on travel time and streamlining care routines, telehealth makes it easier for patients to stick to their treatment plans, ultimately improving how metabolic syndrome is managed.
How do Bluetooth-enabled devices help with remote health monitoring?
Bluetooth-enabled devices make remote health monitoring much more convenient by automatically sending precise readings to healthcare providers in real time. This removes the hassle of manual data entry, cutting down on errors and allowing for quicker adjustments to treatment plans when needed.
These devices also play a big role in keeping patients engaged and committed to their care. By simplifying progress tracking and maintaining a direct link with clinicians, they encourage better adherence to health routines. This is particularly helpful for managing conditions like metabolic syndrome, where regular monitoring and timely interventions are key to improving health outcomes.
How do government subsidies help make telehealth more affordable for managing metabolic syndrome?
Government subsidies, including CHAS and MediSave, play a crucial role in making telehealth more affordable for managing metabolic syndrome. These programmes enable patients to use subsidised funds to cover expenses such as video consultation fees, prescribed medications, and essential tests for chronic conditions tied to metabolic syndrome.
With these subsidies, patients can access convenient and reliable telehealth services while keeping out-of-pocket expenses low. This approach not only makes healthcare more accessible but also supports individuals in managing their health more effectively without financial strain.
.png)

