
GLP-1 Eligibility: Common Disqualifiers

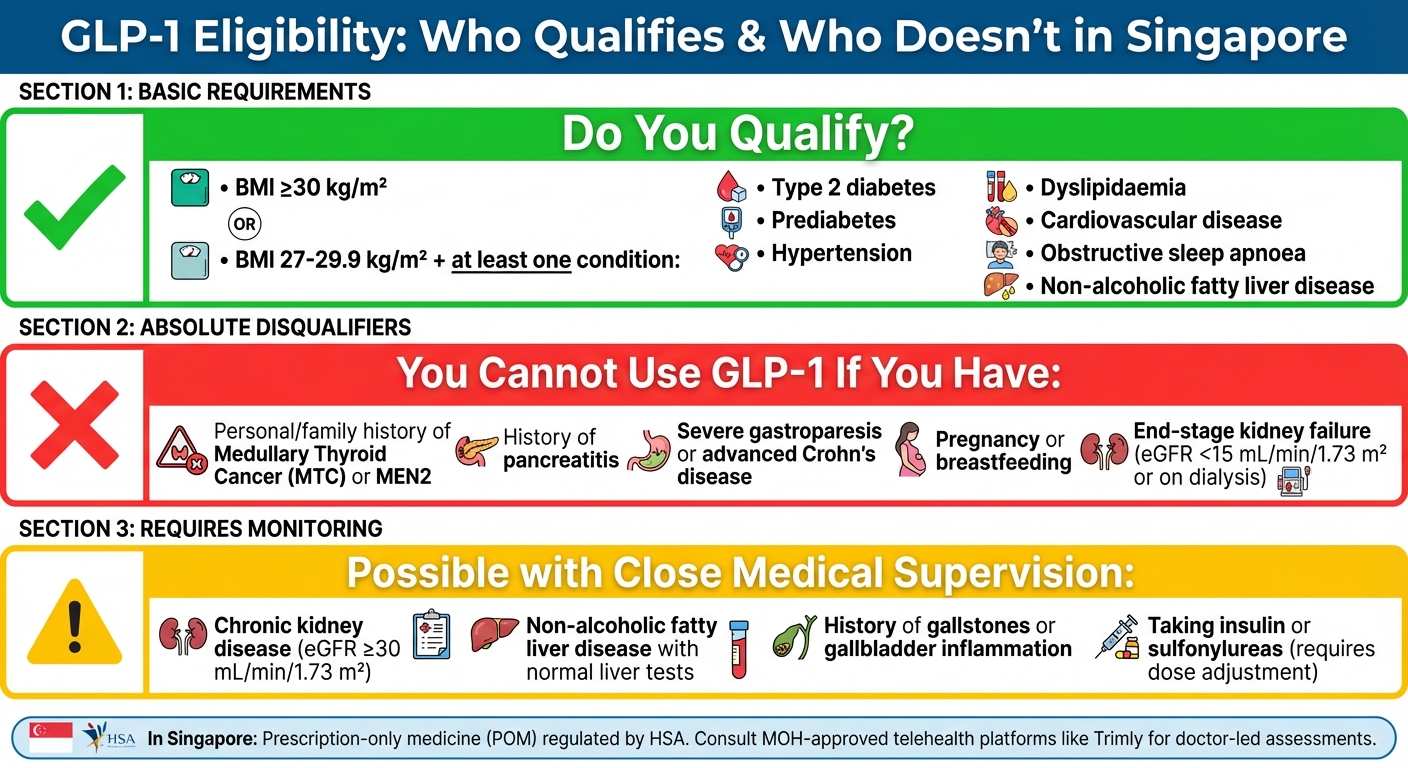
If you're considering GLP-1 medications for weight loss or diabetes, it's crucial to know who qualifies and who doesn't. These drugs, like semaglutide or liraglutide, are effective for managing obesity or type 2 diabetes but come with strict eligibility criteria. Here's what you need to know:
Key Disqualifiers:
- Medullary Thyroid Cancer (MTC) or MEN2: Personal or family history excludes you due to potential thyroid risks.
- Pancreatitis: A history of this condition makes GLP-1 unsafe as it can worsen pancreatic inflammation.
- Severe Digestive Issues: Conditions like gastroparesis or advanced Crohn’s disease are incompatible due to slowed gastric emptying.
- Pregnancy or Breastfeeding: These medications are not safe during these periods.
- End-Stage Kidney Failure: Patients with an eGFR below 15 mL/min/1.73 m² or on dialysis cannot use GLP-1.
Conditions Requiring Monitoring:
- Chronic Kidney or Liver Disease: May be possible with close observation.
- Gallbladder Issues: A history of gallstones or inflammation needs careful review.
- Other Diabetes Medications: Combining GLP-1 with insulin or sulfonylureas requires dose adjustments to avoid hypoglycaemia.
In Singapore, GLP-1 medications are prescription-only and regulated by the Health Sciences Authority (HSA). Platforms like Trimly offer telehealth consultations with local doctors to assess eligibility and provide personalised treatment plans. Always consult a licensed doctor to determine if GLP-1 is right for you.
GLP-1 Medication Eligibility Requirements and Disqualifiers in Singapore
Basic Requirements for GLP-1 Medications
BMI and Health Condition Requirements
In Singapore, eligibility for GLP-1 medications is guided by specific BMI and health condition criteria. To qualify, patients must have a BMI of 30 kg/m² or higher. Alternatively, those with a BMI between 27 and 29.9 kg/m² may also qualify if they have at least one weight-related health condition. These conditions include type 2 diabetes, prediabetes, hypertension, dyslipidaemia, cardiovascular disease, obstructive sleep apnoea, or non-alcoholic fatty liver disease.
Clinical trials for GLP-1 medications did not include participants with a BMI below 27 kg/m² due to limited safety data and a higher likelihood of side effects at lower weights. These eligibility criteria are designed to ensure that the medications are both safe and effective for individuals who meet the outlined thresholds.
Diabetes Treatment vs. Weight Loss Use
GLP-1 medications are approved for different purposes depending on the drug and dosage. For example, Ozempic (semaglutide 0.5–1 mg) is primarily used to manage type 2 diabetes. It helps control blood sugar levels and reduces cardiovascular risks. On the other hand, Wegovy (semaglutide 2.4 mg) and Saxenda (liraglutide 3 mg) are specifically approved for long-term weight management in adults who meet the BMI and health condition criteria.
When prescribed for diabetes, factors like HbA1c levels, cardiovascular risks, and kidney function often influence the choice of GLP-1 medication. For weight management, doctors assess whether patients meet the BMI requirements and whether prior efforts, such as diet and exercise, have failed to produce significant results. These distinctions are important for ensuring appropriate use under Singapore’s medical regulations.
Singapore's Prescription Rules
In Singapore, GLP-1 medications are classified as prescription-only medicines (POM) by the Health Sciences Authority (HSA). This means they can only be obtained through consultation with a doctor registered with the Singapore Medical Council. Telehealth platforms approved by the Ministry of Health, such as Trimly, offer doctor-led assessments and home delivery services for these medications when deemed suitable.
The prescription process in Singapore includes calculating BMI using metric measurements (weight in kilograms divided by height in metres squared), conducting blood tests to check kidney and liver function, and screening for any contraindications. While the local guidelines align with international standards, they also take into account Singapore’s specific public health goals and priorities.
Medical Conditions That Prevent GLP-1 Use
Medullary Thyroid Cancer or MEN2
If you or your family have a history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2), GLP-1 medications are off the table. This restriction is no small matter - it’s highlighted in boxed warnings by regulatory bodies like the FDA and Singapore's Health Sciences Authority. Why? Rodent studies have shown that high doses of GLP-1 medications can lead to thyroid C-cell adenomas in about 5–10% of cases. While it’s unclear if this applies to humans, the risk is significant enough that doctors in Singapore routinely screen for these conditions before prescribing GLP-1 treatments. It’s a precaution worth taking seriously.
Pancreatitis
If you’ve had pancreatitis before - especially recurrent or unexplained episodes - GLP-1 medications are not an option. Pancreatitis, an inflammation of the pancreas, has been linked to a higher risk when using these medications. For instance, clinical trials reported acute pancreatitis in 0.1–0.2% of patients on semaglutide, compared to none in placebo groups. Post-marketing data suggests the rates could be even higher. Since GLP-1 treatments slow down gastric emptying and affect pancreatic secretions, they can trigger severe flare-ups that might land you in the hospital. Medications like Ozempic, Wegovy, and Saxenda explicitly list a history of pancreatitis as a contraindication. If this applies to you, your doctor will carefully review your medical history to avoid any risks.
Severe Digestive System Diseases
Certain gastrointestinal conditions make GLP-1 medications unsafe. For example, gastroparesis, where the stomach empties unusually slowly, is a clear no-go. GLP-1 treatments further delay gastric emptying, which can worsen symptoms significantly. Similarly, severe inflammatory bowel diseases like advanced Crohn's disease or ulcerative colitis might also be aggravated by the slowed digestive motility these medications cause. It’s essential to discuss any chronic digestive issues with your doctor during your consultation to ensure these medications are suitable - or not - for you.
Pregnancy and Breastfeeding
Pregnancy and breastfeeding are absolute contraindications for GLP-1 medications. While no human trials have been conducted for ethical reasons, animal studies suggest these treatments may cause embryofetal toxicity. Women planning to conceive are advised to stop GLP-1 treatments at least two months before trying to get pregnant, allowing enough time for the medication to clear from the body. If you become pregnant while on GLP-1 therapy, you should discontinue it immediately and consult your doctor. Since there’s also no data on whether these medications pass into breast milk, breastfeeding mothers are encouraged to explore alternative options for weight management.
End-Stage Kidney Failure
For patients with end-stage kidney disease, GLP-1 medications are not an option. This typically applies to those with an estimated glomerular filtration rate (eGFR) below 15 mL/min/1.73 m² or those on dialysis. Clinical trials generally excluded individuals with severe kidney issues due to concerns about reduced medication clearance. Additionally, common side effects like nausea, vomiting, and diarrhoea can lead to dehydration, further straining kidney function. Doctors routinely assess kidney health using eGFR tests, and severe impairment rules out GLP-1 treatments. Telehealth platforms approved by Singapore’s Ministry of Health, such as Trimly, also require these screenings before issuing prescriptions.
GLP-1 RAs: When Not to Prescribe
sbb-itb-5db499f
Conditions Requiring Extra Monitoring
While the conditions outlined below don't automatically rule out patients from receiving GLP-1 therapy, they do call for closer observation and careful dose adjustments. This is a key part of Singapore's evaluation process for determining GLP-1 eligibility.
Chronic Kidney or Liver Disease
For patients with chronic kidney disease (CKD) (eGFR ≥30 mL/min/1.73 m²) or non-alcoholic fatty liver disease (NAFLD) with normal liver test results, GLP-1 therapy can typically proceed with regular baseline and follow-up assessments. Most GLP-1 drugs don’t require dose changes at this stage, but it’s crucial to monitor kidney function, especially after dose adjustments or if symptoms like vomiting, diarrhoea, or reduced fluid intake arise. For instance, a patient with type 2 diabetes, a BMI of 33, and stage 3a CKD might start on a low dose, with quarterly reviews and hydration advice included in their care plan.
In contrast, for those with moderate to severe cirrhosis, doctors exercise greater caution due to concerns about drug metabolism and the risk of liver decompensation. Baseline liver function tests - such as ALT, AST, bilirubin, and albumin - are usually conducted, with follow-ups if symptoms like nausea, abdominal swelling, or jaundice appear. Other pre-existing conditions may also require tailored monitoring protocols.
History of Gallbladder Problems
A history of gallstones or gallbladder inflammation doesn’t necessarily exclude someone from GLP-1 therapy but does require closer observation. Clinical studies have shown a slightly increased likelihood of gallbladder issues, likely tied to rapid weight loss and changes in gallbladder motility. For example, in the STEP programme for semaglutide, gallbladder-related events occurred in 2.6% of participants compared to 1.2% in the placebo group. Doctors will typically review your medical history and advise you on warning signs like right-upper-quadrant abdominal pain, fever, or jaundice. If symptoms are present, a baseline abdominal ultrasound may be recommended. Local telehealth services often assist in this process by using structured follow-up questionnaires to track symptoms.
Use with Other Diabetes Medications
When GLP-1 medications are combined with other diabetes treatments, interactions need extra attention. On their own, GLP-1 drugs rarely cause severe hypoglycaemia since their insulin-stimulating effect is glucose-dependent. However, combining them with insulin or sulfonylureas (like glipizide, gliclazide, or glimepiride) can significantly increase the risk of hypoglycaemia - up to tenfold if no dose adjustments are made. To reduce this risk, doctors often suggest lowering the initial dose of these medications, particularly if your HbA1c levels are already close to the target range. For basal insulin, an initial reduction of around 10–20% is common, with further adjustments based on blood sugar readings. Patients are encouraged to monitor their blood sugar levels more frequently during the first one to two weeks and report symptoms of low blood sugar - such as shakiness, sweating, or confusion - so that their treatment can be promptly adjusted.
GLP-1 Regulations and Practices in Singapore
How Singapore Regulates GLP-1 Medications
In Singapore, medications like liraglutide, semaglutide, and dulaglutide - part of the GLP-1 receptor agonist class - are strictly regulated as prescription-only drugs under the Health Products Act. The Health Sciences Authority (HSA) carefully reviews these medications for safety, quality, and effectiveness before approving them for specific uses, such as managing type 2 diabetes or aiding in chronic weight management. To ensure prescribing practices align with the latest evidence, the Ministry of Health (MOH) provides detailed guidelines.
Enforcement by the HSA is stringent. Regular actions such as product seizures and fines underscore the importance of compliance. Additionally, post-marketing surveillance is mandatory to monitor adverse effects, which could include pancreatitis, gallbladder issues, or severe gastrointestinal side effects [5, 7]. These measures ensure that patients in Singapore have access to safe and well-regulated GLP-1 treatments.
Accessing GLP-1 Through Telehealth
Telehealth has become a convenient option for accessing GLP-1 medications, thanks to MOH-licensed platforms. With the Healthcare Services Act (HCSA) fully in effect as of 2023, telemedicine is now a regulated healthcare service in Singapore. This framework requires proper medical evaluations, comprehensive documentation, informed patient consent, and continuity of care.
An example is Trimly, an MOH-approved telehealth clinic. Through video consultations, Singapore-registered doctors assess patients by reviewing factors like BMI, comorbidities, medication history, and potential contraindications before issuing e-prescriptions. Dr. Zac Yeo, Medical Director at Trimly, explains:
"Every prescription decision is made by a licensed doctor after reviewing your health, meds and goals."
After a prescription is issued, licensed pharmacies handle the dispensing and delivery of medications. Trimly also offers patients free, unlimited follow-ups to monitor progress and make necessary dose adjustments [2, 4]. This structured approach reflects international best practices, giving patients confidence in the system.
Applying International Guidelines in Singapore
Singaporean clinicians incorporate global research findings into local practices to refine treatment protocols. For instance, Trimly draws on data from the STEP 1 trial published in the New England Journal of Medicine in 2021. This study demonstrated that adults using Wegovy® (semaglutide 2.4 mg) alongside diet and exercise achieved an average weight loss of approximately 15% over 68 weeks.
Local adaptations of international guidelines also consider unique regional factors. For example, Singapore recognises that Asian populations often face higher cardiometabolic risks at lower BMI thresholds. As a result, MOH institutions may apply stricter criteria for subsidised treatments to account for budgetary constraints. Additionally, Singapore adheres to global contraindication standards, including exclusions for individuals with a personal or family history of medullary thyroid carcinoma, MEN2, severe pancreatitis, significant gastrointestinal motility disorders, or known hypersensitivity to these medications.
This integration of global and local practices ensures tailored, effective, and safe care for patients in Singapore.
Conclusion
Main Disqualifiers to Remember
While GLP-1 medications offer promising benefits, certain conditions make their usage unsuitable. If you have a personal or family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia type 2 (MEN2), GLP-1s are not recommended due to the associated risk of thyroid C-cell tumours. Similarly, a history of pancreatitis is an absolute contraindication, as these medications may exacerbate pancreatic inflammation. Those with severe gastroparesis or significant gastrointestinal motility disorders should also steer clear, as GLP-1s slow gastric emptying, potentially worsening these conditions. Women who are pregnant, breastfeeding, or planning to conceive should avoid these medications. Lastly, individuals with end-stage kidney failure (e.g., requiring dialysis) are generally advised against GLP-1 use.
In some cases, conditions may not entirely disqualify you but do require careful monitoring. For example, patients with mild kidney or liver impairments may still be eligible, provided they are closely supervised. However, those with a history of pancreatitis combined with gallbladder issues often do not qualify. These nuances underline the importance of consulting a healthcare professional before starting GLP-1 therapy.
Getting Professional Medical Advice
Because of the complexities involved, it’s essential to seek advice from a licensed doctor who can assess your full medical history, test results, and current medications. Self-assessment is not sufficient - only a qualified healthcare provider can determine if GLP-1 medications are safe and appropriate for you.
In Singapore, Trimly, an MOH-approved telehealth clinic, provides a convenient and professional option for accessing personalised weight loss care. Through video consultations, Singapore-registered doctors evaluate factors like BMI, comorbidities, and medical history to determine eligibility for GLP-1s. If prescribed, medications are delivered directly to your home, and free, unlimited follow-ups ensure your progress is monitored and doses adjusted as needed. Avoid sourcing GLP-1s from unverified online platforms or overseas sellers without a valid local prescription, as this poses serious health and regulatory risks.
For those who are not suitable candidates for GLP-1s, there are still effective alternatives. Doctors can recommend tailored lifestyle programmes, other medications, or referrals to specialists such as dietitians, psychologists, or bariatric experts. Many individuals achieve lasting weight loss through these non-GLP-1 methods, especially when supported by a structured, evidence-based approach.
FAQs
What medical conditions could make someone ineligible for GLP-1 medications?
Certain medical conditions can make GLP-1 medications unsuitable for some people. For instance, if you have a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia type 2 (MEN 2), these medications are not recommended. Similarly, individuals with severe gastrointestinal issues like gastroparesis or a history of pancreatitis should steer clear of these treatments.
Additionally, if you've had allergic reactions to GLP-1 drugs in the past, using them could pose a risk. It's essential to consult your doctor to assess whether these medications are suitable for you, based on your medical history and current health condition.
What is the difference between using GLP-1 medications for diabetes and for weight loss?
GLP-1 medications are versatile, with their effects tailored to different health goals. For diabetes management, they focus on regulating blood sugar levels. They achieve this by improving the body's response to insulin and reducing the amount of glucose produced by the liver. On the other hand, when prescribed for weight loss, these medications take a different approach. They help by curbing appetite, slowing down digestion, and adjusting metabolic processes to aid in steady and manageable weight reduction.
Although these medications belong to the same class, their purpose and expected results vary depending on an individual's health needs. It's essential to consult a doctor to determine the most appropriate treatment for your specific condition.
Why should I consult a healthcare professional before starting GLP-1 medication?
Consulting a healthcare professional is crucial to determine if GLP-1 medication is the right choice for you. They’ll carefully review your medical history, assess any existing conditions or potential risks, and create a treatment plan tailored specifically to your needs.
This personalised approach not only reduces the chances of side effects but also ensures the medication supports your overall health and weight management goals. Relying on expert advice is key to achieving safe and effective outcomes.
.png)

