
How Digital Literacy Shapes Telehealth in Singapore

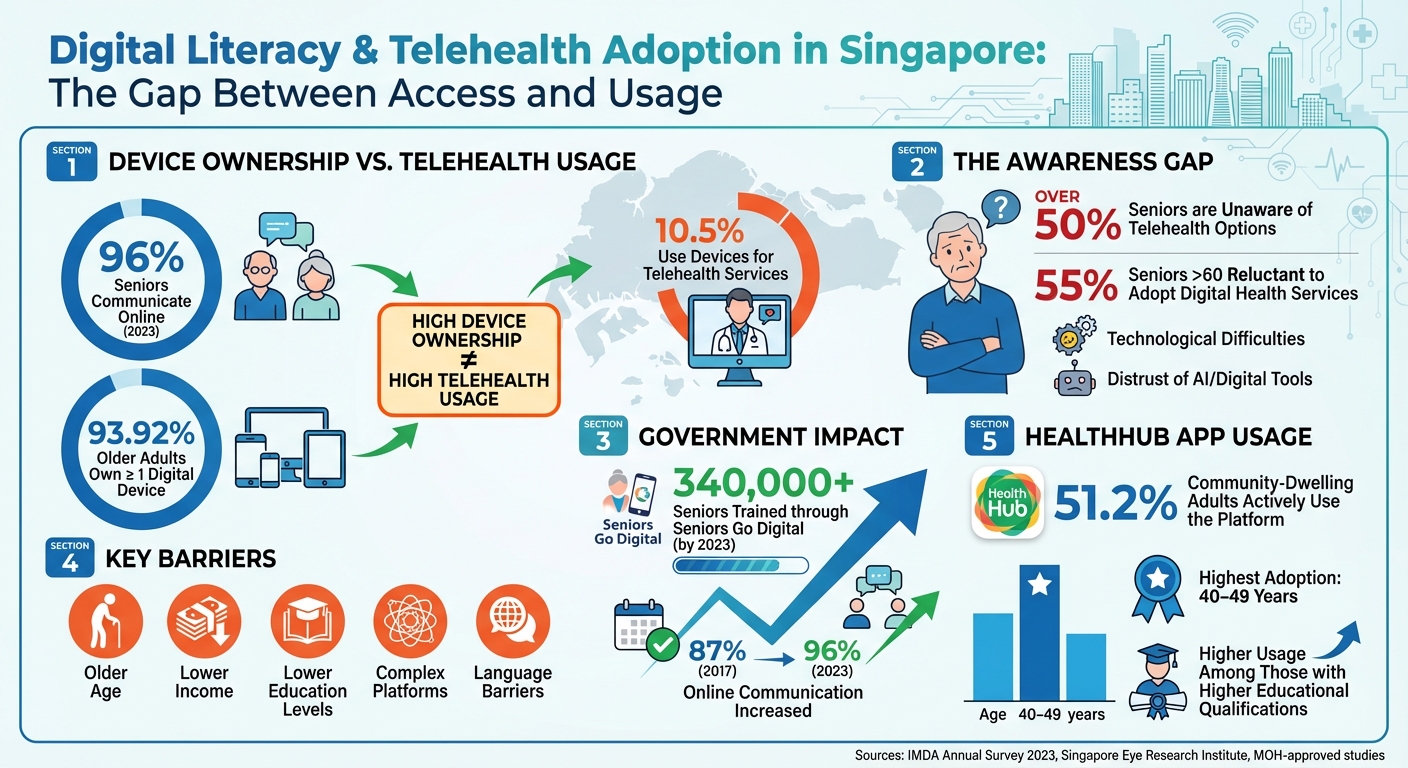
Digital literacy is now a key factor in accessing healthcare in Singapore. While most people own devices and have internet access, using telehealth services remains low, especially among seniors and lower-income groups. Government programmes like Seniors Go Digital and Digital for Life aim to bridge this gap, training over 340,000 seniors by 2023. However, only 10.5% of seniors use telehealth services, with barriers like skill gaps, complex platforms, and a lack of awareness being common.
Key findings include:
- Older age, lower income, and education levels reduce telehealth adoption.
- 55% of seniors above 60 are reluctant to use digital health tools, citing trust and technical issues.
- Simplified platforms, multilingual support, and regular training improve accessibility.
Telehealth services, such as MOH-approved clinics like Trimly, show how user-friendly design can ease adoption. These platforms offer online consultations and medication delivery but require digital proficiency. Improving digital literacy and platform usability is critical for making telehealth more accessible across Singapore.
Digital Literacy and Telehealth Adoption in Singapore: Key Statistics
Digital Literacy Levels in Singapore: Current State
National Surveys and Digital Literacy Programmes
Singapore presents an interesting digital paradox: while nearly everyone has access to devices and the internet, the use of digital health tools remains surprisingly low. According to IMDA's Annual Survey on Infocomm Usage, 96% of seniors were communicating online in 2023, a notable improvement from 87% in 2017. This progress highlights the success of initiatives like Seniors Go Digital and Digital for Life, which focus on teaching practical skills such as using messaging apps, navigating mobile interfaces, and online safety.
However, connectivity doesn’t necessarily translate to digital health readiness. While many older adults can now send WhatsApp messages or browse the internet, only 10.5% report using telehealth services on their devices. Even more concerning is that over half of seniors are unaware of telehealth options. A study on the HealthHub app in 2025 revealed that only 51.2% of community-dwelling adults actively used the platform, with higher adoption rates among those aged 40–49 years and individuals with higher educational qualifications. These numbers highlight the need to better understand the challenges faced by specific groups.
Barriers Faced by Specific Population Groups
Certain groups face more pronounced challenges in digital health literacy: seniors (especially those over 60), lower-income households, and individuals with lower education levels. Research indicates that digital health literacy tends to decline with age and is positively associated with having a mobile phone data plan. A survey by the Singapore Eye Research Institute found that 55% of seniors above 60 were unlikely to adopt digital health services, citing issues like technological difficulties and distrust of AI and digital tools as key reasons.
The challenges aren’t limited to seniors. Studies on telemedicine adoption show that older age, lower income, and lower education are linked to reduced acceptance and adherence to telehealth services. For example, platforms like Trimly, which provide personalised GLP-1 treatments and video consultations, are easily accessible to younger, employed, and tech-savvy individuals. However, older or lower-income users often struggle with tasks like completing online medical forms or navigating e-consent processes, making it harder for them to benefit from telehealth platforms.
Government Programmes to Improve Digital Literacy
To tackle these barriers, the government has rolled out targeted interventions. The Seniors Go Digital programme, launched in May 2020, provides affordable devices, data plans, and step-by-step digital guidance. A study involving 138 digitally excluded older adults aged 55 and above from lower socioeconomic backgrounds found that providing smartphones, cellular data, and regular digital literacy training (fortnightly to monthly) significantly improved their digital skills and reduced social isolation.
While these efforts have laid an important foundation, there’s still a gap in health-specific training. Seniors may now feel confident communicating online, but they need hands-on practice for tasks like booking telehealth appointments or managing digital health records. Policymakers are increasingly recognising that consistent training is more effective than one-off workshops, especially when dealing with complex health management tasks that require ongoing engagement and multiple steps.
Research Findings: Digital Literacy and Telehealth Adoption
How Digital Literacy Affects Telehealth Adoption Rates
In Singapore, research consistently highlights a strong link between digital literacy and the willingness to embrace telehealth. Put simply, higher digital skills make people more open to trying telehealth, while limited skills often act as a roadblock. A cross-sectional study focusing on telemedicine use among older adults revealed that factors like older age, lower education levels, and lower household income were tied to reduced acceptability, desirability, and adherence (ADA) to telemedicine. This was true even after accounting for variables like gender and chronic health conditions.
This creates a noticeable divide: working-age adults, who tend to have better education and more exposure to technology, view telehealth as a natural extension of their digital habits. On the other hand, individuals with lower digital literacy face significant hurdles in adopting these services.
Community research further shows that digital health literacy tends to decline with age, with adults who regularly use mobile data plans demonstrating better skills. This gap is particularly stark among seniors. According to a survey by the Singapore Eye Research Institute, 55% of seniors over 60 were reluctant to adopt digital health services, citing challenges with technology and a lack of trust in digital tools.
User Experience and Treatment Adherence in Telehealth
Digital literacy doesn’t just influence whether someone tries telehealth - it also shapes their ongoing experience. People with stronger digital skills report smoother interactions and higher satisfaction, while those with limited skills often feel stressed, confused, or mistrustful. For older adults, navigating health apps and portals can be especially frustrating, with issues like small fonts or unfamiliar terms adding to the challenge. Even technical glitches, like dropped video calls, can reinforce the idea that telehealth is unreliable, further eroding trust among users with lower digital proficiency.
Limited digital skills can disrupt adherence at multiple stages of the telehealth process. For example, older adults with lower literacy often miss follow-up appointments or medication reminders because they don’t know how to check app notifications, manage SMS alerts, or join scheduled video consultations. In the earlier-mentioned study on telemedicine among older adults, those with lower education and income levels were less likely to maintain consistent telehealth routines or follow through with teleconsultations.
Case Studies and Population Patterns
Real-world examples clearly show how gaps in digital skills affect telehealth usage. A clear age-related trend emerges: younger and middle-aged adults, who generally have better digital literacy, are more likely to adopt telehealth, while seniors report the lowest uptake rates. During Singapore’s first COVID-19 circuit breaker period in May–June 2020, a qualitative study involving 78 elderly participants (average age 73) found that over 50% were unaware of telehealth services. Even though 93.92% of older adults owned at least one digital device, only 10.5% used them for telehealth purposes.
One promising approach to bridging this gap comes from a controlled study that focused on "digitally excluded" seniors from lower-income backgrounds. Participants were provided with smartphones, data plans, and regular digital literacy training. Those who received the training showed noticeable improvements in digital skills and online engagement compared to those still awaiting training. These gains helped seniors learn essential skills like messaging, making video calls, and browsing online safely. Additionally, qualitative studies found that seniors who attended community smartphone classes became more confident using health apps and portals. Classes that incorporated real-life health scenarios - like booking appointments or checking test results - were especially effective in building their confidence.
Addressing Usability and Accessibility Barriers in Telehealth
Common Usability Barriers in Telehealth Platforms
Telehealth adoption isn’t without its hurdles, and these often stem from both technical and human challenges. For many users, especially those with limited troubleshooting skills, complex interfaces, multi-step booking processes, and unreliable internet connectivity can make navigating telehealth platforms frustrating. While 38.1% of seniors own one digital device and 55.82% have two or more, only a small portion - 10.5% - actually use these devices for telehealth services.
Language barriers add another layer of difficulty. For instance, research highlights that Chinese seniors often rate telemedicine platforms less favourably because many lack support for their preferred language or fail to account for their cultural context. When instructions are presented solely in English or filled with medical jargon, seniors with lower health literacy may struggle to follow along. Combined with limited digital skills, these language challenges leave over half of older adults unaware of telehealth services altogether. Tackling these technical and linguistic barriers is a key step towards bridging the digital divide in healthcare access.
Closing the Digital Divide in Telehealth
Efforts like the Seniors Go Digital programme are already making strides in this area, providing affordable devices, data plans, and regular training sessions to improve digital engagement. By 2023, more than 340,000 seniors had participated in training, boosting online communication rates from 87% in 2017 to 96%. However, despite these improvements, 55% of seniors over 60 remain hesitant to embrace digital health services, citing persistent technology challenges.
One-off training sessions often aren’t enough. Research suggests that frequent, supervised lessons in a relaxed setting can help older adults gradually build their confidence with technology. For example, a non-randomised study conducted between July 2020 and November 2021 equipped 138 low-income seniors (aged 55 and above) with smartphones, data plans, and regular volunteer-led training. This hands-on approach allowed participants to master essential skills like video calling and messaging, directly enabling them to access telehealth services. Caregiver involvement also plays a critical role, particularly for seniors with chronic conditions or mobility limitations. Beyond addressing the digital gap, attention must also be given to improving platform usability for long-term engagement.
User-Friendly Design Features in Digital Health Tools
To ensure telehealth platforms are accessible, their design must align with users’ digital literacy levels. Features such as mobile-optimised interfaces, clear visual aids, simplified navigation, multilingual support, and culturally relevant instructions can make a significant difference. Instead of overwhelming users with cluttered dashboards, well-designed platforms guide them through each step. For instance, offering fully online services - from booking appointments to home delivery of medications - removes the need to juggle multiple systems or visit physical locations. Additionally, asynchronous communication options, like messaging healthcare providers, can be a more comfortable alternative for users who find live video calls intimidating.
Other thoughtful features include larger fonts, voice guidance, and visual prompts, all of which help users navigate digital health tools with ease. The focus should always be on designing systems that meet users where they are, rather than expecting them to adapt to overly complicated platforms. When platforms are tailored to users' skills, they not only enhance engagement but also contribute to better health outcomes overall.
sbb-itb-5db499f
Digital Literacy in Telehealth Weight Management and GLP-1 Treatments
Digital Literacy Requirements in Telehealth Weight Management
Managing weight through telehealth services, especially with GLP-1 treatments, requires a fair level of digital know-how. Users are expected to navigate online booking systems, fill out medical questionnaires digitally, and, once treatment begins, log personal data like weight, diet, and activity levels to track progress. For those on GLP-1 treatments, understanding dosing schedules, identifying potential side effects, and managing e-prescriptions are also key responsibilities.
A study conducted in Singapore highlighted a concerning trend: older adults with lower education and income levels scored poorly on acceptability, desirability, and adherence (ADA) metrics for telemedicine. Some participants reported acceptability scores as low as 2 out of 25 and adherence scores of just 8 out of 40. Those who struggled with digital navigation and virtual interfaces faced the greatest challenges. This is particularly troubling for weight management programmes, which rely on consistent user engagement. Issues like difficulty entering biometric data or interpreting dashboard visuals can significantly impact adherence to treatment plans. These findings underline the importance of designing user-friendly platforms that cater to varying levels of digital literacy.
The Importance of Simple Platforms for Long-Term Care
For weight management programmes to succeed, platforms must be straightforward and easy to use. Achieving sustainable weight loss often requires ongoing commitment, regular progress updates, and the ability to adjust treatment plans as needed. Complicated interfaces with too many steps or unclear navigation can discourage users, especially those less comfortable with technology.
Trimly, a telehealth clinic approved by Singapore's Ministry of Health (MOH), offers a great example of simplicity in design. Their platform operates on a clear, three-step process: patients book an appointment and complete a medical questionnaire online, consult a doctor via video for personalised GLP-1 treatment options (either oral or injectable), and receive their medication delivered to their doorstep. The service also includes unlimited follow-ups and online messaging support, all within a user-friendly interface.
One patient shared their experience:
"I loved that everything was done online, from consults to follow-ups, so I didn't have to take time off just to see a doctor".
Another patient, Adam, noted the platform's flexibility:
"Being able to chat with the clinic online and adjust my plan when I hit plateaus made a lot of the difference in staying consistent".
Matching Platform Design to User Skills
Telehealth platforms work best when they align with the digital skills of their users. Simple onboarding quizzes, asking about prior experience with apps or video calls, can help customise the interface to meet individual needs. For instance, a "basic mode" could feature larger icons, voice-guided tutorials, and simplified menus for less tech-savvy users, while more advanced users could access detailed analytics and reporting options.
Despite government efforts to boost digital literacy, only 10.5% of older adults in Singapore currently use telehealth services. This highlights the need for platforms that cater to varying skill levels. For weight management services involving GLP-1 medications, essential tasks like booking appointments, viewing treatment plans, logging weight, and ordering refills must be as simple as possible. Features such as multi-language support (English, Mandarin, Malay, Tamil), offline progress logging with automatic syncing, and one-tap access to video consultations can significantly lower barriers. By designing platforms with diverse user needs in mind, telehealth services can not only improve accessibility but also enhance long-term adherence, which is crucial for achieving sustainable weight loss.
Conclusion: Improving Digital Literacy to Advance Telehealth in Singapore
Key Takeaways
Digital literacy plays a pivotal role in ensuring telehealth services are safe, accessible, and effective in Singapore. Studies show that better digital skills lead to higher acceptance, preference, and adherence to telemedicine platforms. For long-term care, such as managing weight with GLP-1 treatments, patients often need to perform recurring tasks like reporting symptoms, monitoring side effects, and refilling prescriptions. To maintain consistent engagement, telehealth platforms must cater to users' digital capabilities. This proves that owning a device alone isn’t enough - platforms must also prioritise usability and simplicity. For example, MOH-approved telehealth providers like Trimly operate entirely online, delivering medication straight to patients' homes. Enhancing digital literacy not only improves user safety and satisfaction but also leads to better health outcomes. These findings highlight the urgent need to address the digital divide.
The Need for Collaborative Action
Addressing the digital divide requires a united effort from various stakeholders. The Government has already made strides with programmes like Seniors Go Digital, which has trained over 340,000 seniors since its launch in May 2020. This initiative has increased online communication rates among seniors from 87% in 2017 to 96% in 2023. However, more targeted measures are needed to ensure inclusivity. Healthcare providers could integrate digital literacy checks during patient registration, offer guided onboarding sessions, and design user-friendly interfaces that cater to diverse age groups and backgrounds. Community organisations can step in by hosting practical telehealth workshops in familiar environments, pairing seniors and lower-income individuals with volunteers for hands-on support. Meanwhile, industry players should focus on creating low-bandwidth platforms with support for local languages.
Tracking metrics such as telehealth adoption rates by demographic, digital health literacy levels, and clinical outcomes like weight management progress can help stakeholders measure the effectiveness of these initiatives. By working together, Singapore can ensure that telehealth services benefit everyone, regardless of their age, education, or income level. This collaborative approach is key to building a more inclusive digital health ecosystem.
Digital literacy: About 250,000 people to benefit from S$3m boost to national fund, workshops
FAQs
How does digital literacy affect seniors' use of telehealth services in Singapore?
Digital literacy is a key factor in how seniors in Singapore engage with telehealth services. When older adults possess solid digital skills, they can effortlessly use online platforms, attend virtual medical consultations, and access essential health resources. This makes telehealth not only more accessible but also more efficient for their needs.
On the other hand, a lack of familiarity with digital tools can pose challenges. Seniors may struggle to understand how to use telehealth platforms or face barriers in accessing services. By providing targeted education and support, these obstacles can be reduced, ensuring telehealth becomes a more inclusive option. This, in turn, enhances the healthcare experience for older adults.
What efforts are being made to enhance digital literacy for telehealth in Singapore?
Singapore has rolled out several efforts to improve digital literacy and ensure telehealth services are easy to use and widely accessible. These measures include government-led programmes, community-based workshops, and nationwide digital skills training sessions designed to help individuals confidently use telehealth platforms.
Public awareness campaigns are also playing a key role, introducing residents to the convenience and advantages of telehealth services. By doing so, more people are empowered to access online healthcare with ease. These initiatives align with Singapore's larger vision of building a society where everyone can benefit from digital advancements.
What challenges do older adults in Singapore face when using telehealth services?
Older adults in Singapore often encounter difficulties when it comes to adopting telehealth services. One key hurdle is limited digital literacy, which can make navigating online platforms a daunting task. Many may struggle with the use of smartphones, tablets, or computers during medical consultations, feeling unsure or lacking confidence in their abilities.
On top of that, physical or cognitive challenges - like poor eyesight or memory lapses - can further complicate their experience with telehealth systems. To help overcome these obstacles, it's crucial to design user-friendly platforms and provide support for improving digital skills. This way, telehealth becomes more accessible and practical for older adults.
.png)

