
7 Common GLP-1 Side Effects and How to Manage Them

GLP-1 medications like Saxenda and Ozempic are widely used in Singapore for weight loss and diabetes management. While effective, they can cause side effects, especially early in treatment. Here's what you need to know:
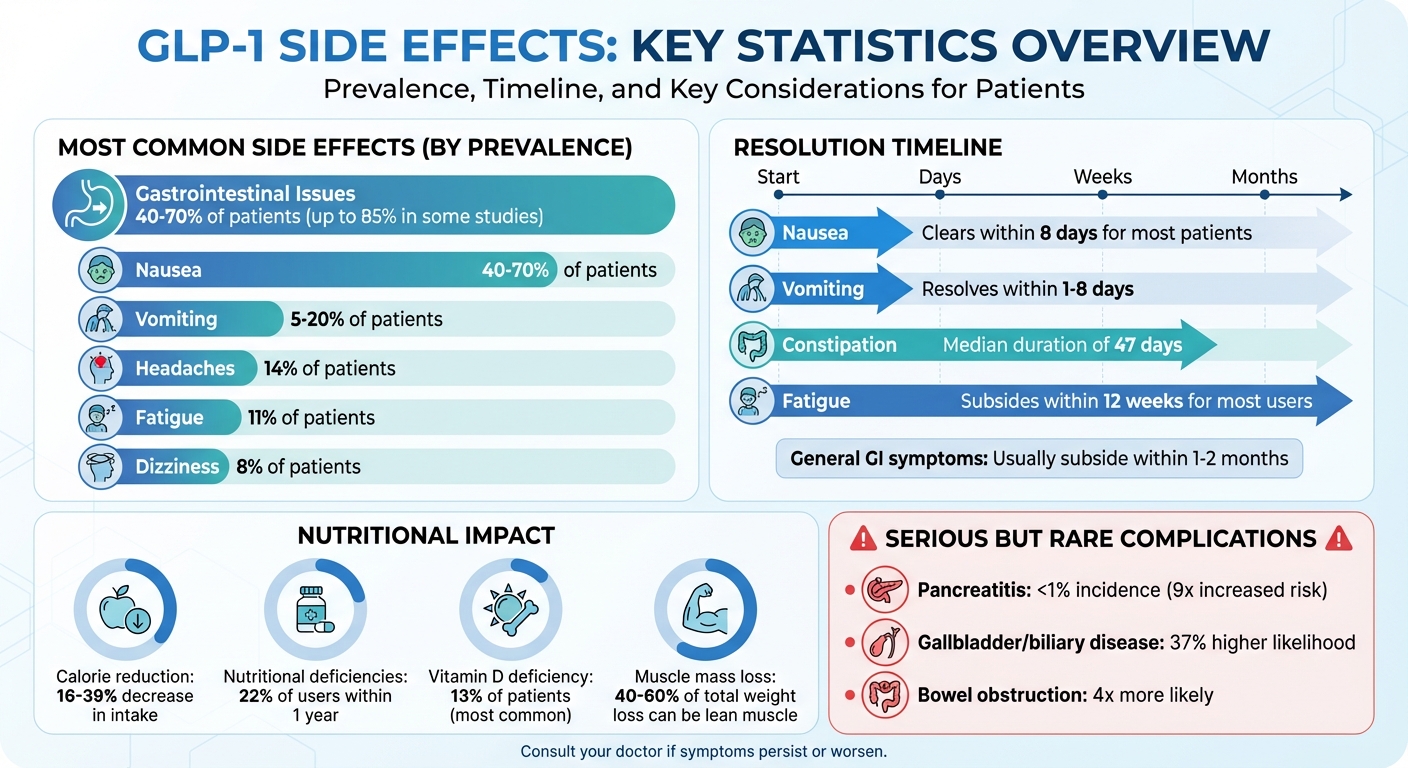
- Common Side Effects: Nausea, vomiting, bloating, constipation, fatigue, headaches, and dizziness are frequent but often mild.
- Why They Occur: These drugs slow stomach emptying and suppress appetite, which can lead to gastrointestinal discomfort and reduced energy intake.
- Management Tips:
- Eat smaller, bland meals to ease nausea.
- Stay hydrated and gradually increase fibre for constipation.
- Monitor calorie and nutrient intake to combat fatigue.
- Adjust doses slowly under medical supervision to minimise side effects.
- Serious Risks: Rare issues like pancreatitis, gallbladder problems, or bowel obstruction require immediate medical attention.
For safe and effective use, consult your doctor regularly and make dietary and lifestyle adjustments. Telehealth services in Singapore can provide convenient follow-ups and guidance.
GLP-1 Medication Side Effects: Prevalence and Timeline
Managing the Gastrointestinal Side Effects of GLP-1s: Focus on Nutrition & Lifestyle Interventions
Nausea and Vomiting: What Causes Them and How to Manage
Nausea is one of the most common side effects of GLP-1 medications, affecting between 40% and 70% of patients at some point during their treatment. Vomiting is less frequent, occurring in about 5% to 20% of cases. The good news? These symptoms are usually mild to moderate and often subside within one to two months as your body gets used to the medication. They tend to appear during the first four to five weeks of treatment or after a dose increase. For most people, nausea clears up within eight days of starting, while vomiting typically resolves within one to eight days.
So, what’s behind these symptoms? There are two key reasons. First, GLP-1 medications slow down how quickly your stomach empties, which means food stays in your stomach longer and can trigger nausea. Second, these medications activate GLP-1 receptors in the brain area responsible for nausea and vomiting. As Micheal Currier, PA-C, explains:
"There are basically two mechanisms that cause nausea. One is due to slowed gastric emptying. GLP1s delay gastric emptying which causes food to sit in the stomach for longer periods of time, which triggers nausea. The other mechanism resides in the central nervous system and is due to how the medication activates GLP-1 receptors in the area of the brain that controls nausea and vomiting, which then leads to an increase in nausea".
With this understanding, there are practical steps and medical strategies to help you manage these symptoms.
Daily Tips to Reduce Nausea
Making small changes to your diet and habits can go a long way in easing nausea. Start by eating smaller meals more frequently instead of sticking to three large ones. Opt for bland, easy-to-digest foods like plain porridge, steamed chicken, or white rice. It’s also a good idea to avoid greasy or high-fat options, as these can be harder on your stomach. Staying hydrated is key - sip water throughout the day to keep your fluid levels up.
Medical Options for Relief
If nausea becomes a challenge, your doctor might adjust your treatment plan. One common approach is starting with a low dose and increasing it gradually, giving your body time to adapt. Micheal Currier, PA-C, highlights this approach:
"Slowly increasing the dose of a GLP-1 medication allows the body time to adjust to the changes that are occurring, especially the slowing of gastric motility. So the key to avoiding the nausea as much as possible is to take the titration phase slowly and allow the body time to acclimate appropriately".
If nausea strikes after a dose increase, your doctor might suggest extending the current dose for an extra two to four weeks or temporarily lowering the dose for a few days. In some cases, anti-nausea medications may also be prescribed under medical supervision. However, if these adjustments don’t improve your symptoms, it’s important to know when to seek professional help.
When to See a Doctor
While most nausea and vomiting can be managed, some symptoms shouldn’t be ignored. Stop your medication and seek immediate medical attention if you cannot keep liquids down or if vomiting persists. Severe or ongoing pain in the stomach, abdomen, or back - especially if accompanied by nausea, vomiting, or fever - could signal pancreatitis and requires urgent care.
Be mindful of signs of gallbladder issues, such as pain in the upper right abdomen, bloating, fever, chills, yellowing of the skin or eyes, or clay-coloured stools. Additionally, vomiting blood or experiencing severe abdominal pain that spreads to your back are red flags that call for urgent medical evaluation. In Singapore, you can consult a doctor through telehealth services for an initial assessment or visit the nearest A&E if symptoms are severe.
Digestive Issues: Bloating, Indigestion, and Constipation
GLP-1 medications often bring along digestive challenges like bloating, indigestion, and constipation. These gastrointestinal side effects are reported in 40% to 70% of patients, with some studies noting rates as high as 85%. While most cases are mild, constipation can be particularly persistent, lasting a median of 47 days. This is often linked to slowed gastric emptying, which can also lead to bloating, indigestion, and irregular bowel movements. Let’s look at some practical dietary and lifestyle tips to help manage these symptoms.
Diet and Lifestyle Changes That Help
Simple changes to your eating habits can ease discomfort significantly. Start by having smaller, more frequent meals and take your time chewing. Avoid foods that are fried, fatty, or spicy, as they can be harder to digest. Carbonated drinks are another culprit for bloating, so it’s best to skip those too. A light walk after meals can support digestion, and staying upright for three to four hours after eating may also help. If bloating is an issue, consider avoiding artificial sweeteners commonly found in sugar-free treats, as they can contribute to gas.
How to Relieve Constipation
Hydration plays a key role in combating constipation. Keep sipping water throughout the day, and if plain water feels dull, try adding a splash of lemon, cucumber slices, or mint for a refreshing twist. Boost your fibre intake gradually by including more whole grains, fruits, and vegetables in your diet. Aim for a daily target of 25 to 35 grams of fibre. As Tonya F. Turner, RDN, Associate Director for Clinical Services at MUSC's Weight Management Centre, explains:
"Hydration is also important to staving off constipation. Often, when patients don't feel hungry, they end up not drinking enough water because it makes them feel overly full".
Light exercise, such as walking, cycling, or swimming, can also encourage regular bowel movements. If these adjustments aren’t enough, your doctor might suggest a fibre supplement like psyllium husk or a stool softener to help.
When to Talk to Your Doctor
While many digestive issues improve with time and lifestyle changes, some symptoms may require medical attention. Reach out to your doctor if bloating, indigestion, or constipation persists or gets worse despite your efforts. Immediate help is necessary if you experience severe vomiting, diarrhoea, blood in your stool or vomit, sudden abdominal pain, or signs of dehydration like dizziness, intense thirst, or dark urine. In Singapore, telehealth consultations are a convenient way to get an initial assessment. For urgent cases, head to the nearest A&E for prompt care.
Fatigue, Headaches, and Dizziness: How to Maintain Your Energy
Managing fatigue, headaches, and dizziness is an essential part of navigating GLP-1 treatments. These side effects are quite common, especially in the initial stages. Statistics show that 11% of semaglutide users report fatigue, 14% experience headaches, and 8% feel dizzy. These symptoms often arise due to a significant drop in calorie intake. The good news? Most users find that fatigue subsides within 12 weeks. Knowing what causes these issues and how to handle them can make the process smoother.
Here’s how you can stay energised, hydrated, and vigilant about your health while on GLP-1 medications.
Staying Energised and Hydrated
GLP-1 medications can reduce calorie intake by 16% to 39%, sometimes dipping below the daily minimum of 1,200 kcal for women and 1,800 kcal for men. This sharp reduction can lead to nutritional deficits, with 22% of GLP-1 users developing deficiencies within a year, most commonly Vitamin D deficiency at 13%. To keep your energy levels steady, aim to eat small, nutrient-rich meals throughout the day. Include lean protein, whole grains, fruits, and vegetables in your diet. A daily intake of at least 60 grams of protein is recommended to help prevent muscle loss.
Singapore’s humid weather makes staying hydrated even more critical. Drink 2–2.8 litres of water daily, using a measured bottle to track your intake. If plain water feels monotonous, add a twist of lemon, cucumber, or mint for flavour. For those experiencing vomiting or diarrhoea, adding electrolytes to your water can help replenish lost minerals. Sleep is equally important - aim for 7–8 hours of rest each night to help your body adjust. Gentle activities like walking can boost your energy without causing strain, but avoid vigorous exercise right after meals to sidestep gastrointestinal discomfort.
Lastly, keep an eye on your blood sugar and blood pressure to catch potential problems early.
Checking for Blood Sugar or Blood Pressure Problems
Fatigue and dizziness can sometimes point to underlying issues. If you’re on other diabetes medications alongside GLP-1s, there’s a risk of hypoglycaemia (low blood sugar). Symptoms like weakness, shaking, sweating, blurred vision, or a rapid heartbeat could be warning signs. Keep glucose tablets or a small juice box handy, and consult your doctor if these symptoms persist. Severe dehydration is another concern, especially for those with chronic kidney disease. As Matthew L. Holt, PharmD, BCPS, explains:
"Not only will dehydration worsen side effects, such as constipation, acute dehydration can significantly harm one's kidneys, especially if he or she is already experiencing the early stages of chronic kidney disease".
When to Get Medical Help
For most people, these side effects improve as their bodies adapt to the medication. However, if fatigue, headaches, or dizziness persist beyond four weeks despite lifestyle adjustments, it’s time to consult your doctor. They can check for nutrient deficiencies or other conditions. Seek immediate medical attention if you experience severe hypoglycaemia symptoms like confusion, difficulty swallowing, or loss of consciousness. Worsening vision is another red flag. For unresolved severe symptoms, prompt medical review is essential. In Singapore, telehealth consultations offer a convenient way to get an initial assessment, but urgent cases should head directly to the nearest A&E.
sbb-itb-5db499f
Fast Weight Loss and Reduced Appetite: Keeping Your Body Healthy
When pursuing rapid weight loss, it’s important to ensure your overall health isn’t compromised. While GLP-1 treatments can lead to a weight reduction of 15–20%, losing weight too quickly can result in the loss of lean muscle mass and nutritional deficiencies. Studies show that 40% to 60% of total weight loss can come from lean muscle mass, and 22% of GLP-1 patients experience nutritional deficiencies within a year. The key is to aim for weight loss that’s not just effective but also sustainable.
Safe Weight Loss Targets
Losing weight too rapidly - defined as more than 1% of body weight per week - can bring about serious health concerns. This kind of rapid reduction is linked to a higher risk of micronutrient deficiencies and can result in 15–25% lean muscle mass loss. Other potential issues include reduced bone density, low energy, and even hair thinning. To avoid these problems, focus on gradual progress that allows your body to adjust without sacrificing essential muscle, bone health, or energy levels.
Getting Enough Nutrients
GLP-1 medications can reduce calorie intake by 16–39%, so it’s crucial to make every meal count. Aim for a protein intake of at least 0.8 g per kg of body weight, or about 20–30 g per meal. In Singapore, this can include dishes like steamed fish, chicken breast, tofu, eggs, or low-sugar Greek yoghurt. Vitamin D deficiency affects 13% of patients within one year, so consider taking 5,000–7,500 IU of Vitamin D3 daily, along with 1,000+ mg of calcium. If a reduced appetite makes it hard to hit protein targets, a protein shake with at least 20 grams of protein and minimal sugar can help. Consulting a registered dietitian early in your treatment is a smart move, as they can help identify and address potential deficiencies. Consistently meeting your nutrient needs is a key part of ensuring your weight loss remains safe and manageable.
Tracking Your Weight Loss
Keeping an eye on your progress is essential for safe weight management. Weigh yourself weekly and watch for signs like rapid weight changes, fatigue, or hair loss. Telehealth platforms make it easy to stay in touch with your doctor through unlimited follow-ups, all from the comfort of home. These regular check-ins allow your healthcare team to adjust your treatment plan as needed and monitor for any nutritional deficiencies. This ongoing support helps ensure your weight loss journey stays on the right track.
Serious Side Effects: Warning Signs to Watch For
While most people handle GLP-1 medications without issues, there are rare but serious complications to be aware of. These include pancreatitis, which has an incidence of less than 1% but comes with a ninefold increased risk, and a 37% higher likelihood of gallbladder or biliary diseases, particularly with higher doses or long-term use. Recognising the warning signs early is crucial.
Symptoms That Need Immediate Attention
If you experience severe, persistent abdominal pain that radiates to your back, jaundice, ongoing nausea and vomiting, fever, or pain in the upper-right side of your abdomen, seek medical attention immediately. These could indicate serious conditions like pancreatitis or gallbladder issues. Additionally, difficulty breathing, swelling of the face, or hives are signs of a severe allergic reaction that requires urgent care.
Be alert for symptoms of bowel obstruction, which is about four times more likely with GLP-1 medications. Warning signs include severe bloating, a firm and distended stomach, inability to pass gas, and difficulty having bowel movements. In September 2023, the FDA updated the Ozempic label to include ileus (intestinal paralysis) as a potential adverse reaction based on post-marketing reports. Other symptoms to watch for include decreased urination, swelling in your legs, or any unusual lumps or changes in your neck. If you notice these, contact your healthcare provider promptly.
How Telehealth Helps Monitor Risks
Given the potential for serious complications, regular monitoring is essential. Telehealth offers a practical way to keep track of your health while minimising risks. Platforms like Trimly provide unlimited follow-up consultations, making it easier to address any concerning symptoms early. These services are particularly helpful in identifying rare but severe reactions quickly.
Under Singapore's Healthcare Services Act, teleconsultations must use real-time, interactive, two-way audio-visual communication. Many telehealth providers also require baseline blood tests to check liver and kidney function before prescribing GLP-1 medications. Regular virtual check-ins allow doctors to monitor your condition, adjust medications as needed, or recommend in-person care if serious symptoms arise. This ongoing support is invaluable for ensuring your treatment remains safe and effective, especially when managing rare complications that need prompt attention.
Conclusion: Managing Side Effects for a Safer Weight Loss Journey
GLP-1 medications can be highly effective for weight management when their side effects are handled thoughtfully. Approaches like slowly adjusting dosages, making dietary tweaks, staying hydrated, and adopting healthier lifestyle habits play a crucial role. Educating patients about potential discomfort and when to seek medical advice ensures they are better prepared for the process. Support from healthcare providers, nutritionists, and pharmacists adds another layer of guidance, helping to optimise results.
In addition to self-care, remote support can make a big difference. Platforms like Trimly offer easy access to continuous care. With Trimly, you can schedule personalised follow-up consultations to address any concerns as they come up. Its MOH-approved doctors provide close monitoring, explain possible risks and benefits, and offer tailored advice on diet and lifestyle adjustments.
FAQs
What can I do to reduce nausea and vomiting from GLP-1 medications?
To help with nausea and vomiting, consider having smaller meals more frequently instead of three large ones. Steer clear of greasy, fried, or spicy dishes, as these can irritate your stomach. Staying hydrated is key - take small sips of water throughout the day to avoid dehydration. Natural options like ginger or peppermint may also provide some relief. If your symptoms don't improve or get worse, it's best to reach out to your healthcare provider for tailored guidance.
What serious side effects of GLP-1 medications should I watch out for?
If you're taking GLP-1 medications, it's crucial to be aware of symptoms that might indicate serious side effects needing immediate medical attention. Watch out for:
- Intense or persistent pain in your stomach, abdomen, or back
- Nausea or vomiting that doesn't go away
- Fever or yellowing of your skin or eyes, which could signal liver problems
- Trouble breathing or swallowing
- Swelling in areas like your face, lips, tongue, or throat
- Severe allergic reactions, including rashes, itching, or dizziness
Should you notice any of these signs, don't delay - reach out for medical assistance to prioritise your health.
How can I maintain proper nutrition while on GLP-1 medications for weight management?
To maintain proper nutrition while on GLP-1 medications, try eating smaller, more frequent meals. This approach can help with digestion and reduce any discomfort. Steer clear of greasy or overly spicy foods, as they might worsen nausea, and make sure to stay hydrated throughout the day. If you're adding more fibre to your diet to aid digestion, do it gradually to avoid bloating.
Focus on a balanced and diverse diet that includes plenty of fruits, vegetables, lean proteins, and whole grains to meet your nutritional needs. If digestive issues arise, natural options like ginger or peppermint may help soothe symptoms. For advice tailored to your unique situation, it's a good idea to consult a healthcare professional who can provide specific dietary recommendations based on your health goals.
.png)

